The monitoring and measurement of vital signs and clinical assessment are core essential skills for all healthcare practitioners who work with assigned patients. Acute deterioration in critically ill patients is frequently preceded by abnormal vital or other physiological signs, such as pulse, blood pressure, temperature and respiratory rate. If these changes in the patient’s vital parameters are recognized early, excess mortality and serious adverse events (SAEs) such as cardiac arrest may be prevented.
DEFINITION
The Early Warning Score (EWS) is a scoring system which assists with the detection of physiological changes and may help identify patients at risk of further deterioration. Scores were developed in the late 1990s when studies showed that in-hospital deterioration and cardiac arrest was often preceded by a period of increasing abnormalities in the vital signs.
SCORING SHEET
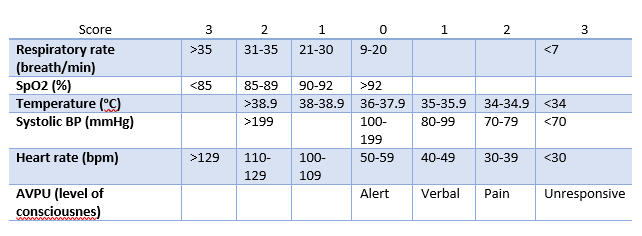
The resulting observations are compared to a normal range to generate a single composite score, for instance based on the following diagram:
A score of five or more is statistically linked to increased likelihood of death or admission to an ICU (Intensive Care Unit). Within hospitals, the EWS is used as part of a "track-and-trigger" system whereby an increasing score produces an escalated response varying from increasing the frequency of patient’s observations up to urgent review by a rapid response or Medical Emergency Team. Concerns by nursing staff may also be used to trigger such call, as concerns may precede changes in vital signs.
MEASUREMENT AND DOCUMENTATION OF OBSERVATIONS
Observations should be taken on all patients admitted to an acute hospital. For every patient, a clear monitoring plan should be developed and documented, that specifies the observations to be recorded and the frequency of observations, considering the patient’s diagnosis and proposed treatment.
The frequency of observations should be consistent with the clinical situation and history of the patient. In the hospital setting, the minimum standard for the assessment of vital signs – utilizing the NEWS (National Early Warning Score) parameters – is every 12 hours. The frequency of patient observations must be reconsidered and modified according to changes in the patient’s clinical condition. This should be documented in the monitoring plan and detailed in the medical notes and nursing care plan. This decision should be made in collaboration between nursing staff and the medical team.
Nursing staff will collect data while performing routine duties. Demographic details, systolic blood pressure, pulse rate, temperature, respiratory rate and AVPU score (A for ‘alert’, V for ‘reacting to vocal stimuli’, P for ‘reacting to pain’, U for ‘unconscious’) are recorded on admission.
Blood pressure and pulse rate are measured electronically and checked manually where appropriate. The temperature is taken orally. The respiratory rate is counted over a full minute. AVPU scores are scored according to best response at time of blood pressure measurement.
Nursing staff will collect physiological parameters twice daily on a dedicated data collection sheet for up to 5 days. Completeness of data is checked daily at the bedside by two of the investigators. The collected data are used to calculate a modified Early Warning Score (as shown above). It is decided from previous experience to define a modified Early Warning Score of five or more as a ‘critical score’. The highest score reached during admission was labelled ‘ScoreMax’.
idsMED provides an Intensive Care solutions for use in ICU, NICU/PICU, ER/A&E. Due to the highly critical conditions in ICU, our devices are equipped with sophisticated alarm systems and smart algorithms to ensure accurate information derived from patient’s vital signs are displayed and calculated correctly with user friendly operations and visualizations. Click here for more information.
Reference: